Rosacea
What is Rosacea?
It is a chronic inflammatory skin condition causing central redness of the face, flushing and texture irregularity of the skin, pustules and red bumps. Long-term eventually leads to permanent thickening (phyma and rhinophyma) and scarring of the central facial regions if not properly treated and controlled. There are four types of rosacea that are classified below.
Type 1
Vascular Rosacea
Inflammatory Rosacea
Phymatous Rosacea
Ocular Rosacea
The problem is not just skin health being adversely affected but very importantly the adverse cosmetic appearance of facial redness, bumps, acne like lesions and thickened texture that it causes.
This inevitably leads to a loss of self-confidence and significant psychological trauma in Rosacea sufferers. Rosacea affects on the centre of the face as such it is difficult to conceal and rosacea is very visible as a result. This makes it an extremely distressing condition to suffer with. The ramifications on self-confidence, body image perception and psychosocial distress are very real and often underplayed.
Why is It Not Effectively Dealt With by the NHS?
Dermacne is proud of the UK healthcare system and it has long been a beacon of free access high quality healthcare for the nation. Unfortunately, due to macroeconomic issues it is becoming more difficult to access treatment for patients. This is due to many factors such as cost, availability of doctors, pressures on the healthcare system etc. The reality is that prevalent skin conditions such as rosacea and acne are not seen as vital concerns by the NHS. As a result, they are not prioritised or addressed.
All dermatologists are aware of the efficacy of oral isotretinoin in rosacea and there is evidence to support this statement. In the UK and in many other developed countries oral isotretinoin is a drug that requires consultant dermatology referral to initiate. As a powerful drug with side effects and moreover teratogenic effects (will cause significant deformity of a fetus/developing baby in any pregnancy that occurs whilst a female patient is on isotretinoin). This is why patients on the medication need to be monitored and also it is extremely important to make sure female patients on oral isotretinoin treatment do not fall pregnant.
This means that there is a significant burden to the already pressured NHS healthcare system due to the monitoring and regulatory requirements of oral isotretinoin as a drug. This means that it is unintentionally but effectively passively withheld from patients that legitimately will benefit due to the pressures on the NHS. With wait times for this being up to 24 months for acne let alone rosacea) it is virtually impossible for the average UK moderate to severe rosacea sufferer that may require oral isotretinoin therapy to get effective long-term management of their condition via the NHS dermatology service.
At Dermacne we believe it is important to provide an alternative and effective pathway for UK patients who have not been able to secure any effective long-term management of their rosacea through the NHS.
Dermacne wishes to provide effective UK regulatory compliant oral isotretinoin therapy for patients who cannot access NHS dermatology services for management of more severe forms of rosacea and rhinophyma.
Dermacne exists as a private service that provides medical evidence-based therapy which is UK guideline compliant for patients who may require more advanced management solutions of their skin condition with oral isotretinoin therapy.

Oral Isotretinoin Therapy in Rosacea.
Off-label means that although the medication does not carry an official license for treatment of rosacea it is recognised as a valid treatment for this dermatological condition by dermatologists.
Which Type of Rosacea is Oral Isotretinoin Useful For?
The following list is a list of the 4 types of Rosacea that are recognised in dermatology.
Oral isotretinoin is an off-label but highly effective treatment in Type 2 – Inflammatory Rosacea (often termed acne rosacea but incorrectly as the spots are not acne but actually what we as dermatologists call inflammatory papules)
Oral isotretinoin is an off-label but highly effective treatment in Type 3 – Phymatous Rosacea (associated with skin thickening and rhinophyma nose skin thickening)
Type 2 – inflammatory rosacea: As well as facial redness, there are red bumps (papules) and pus-filled spots (pustules).
Type 3 – phymatous rosacea: The skin thickens and may become bumpy, particularly on the nose.
Medical Evidence of Oral Isotretinoin Therapy in Rosacea
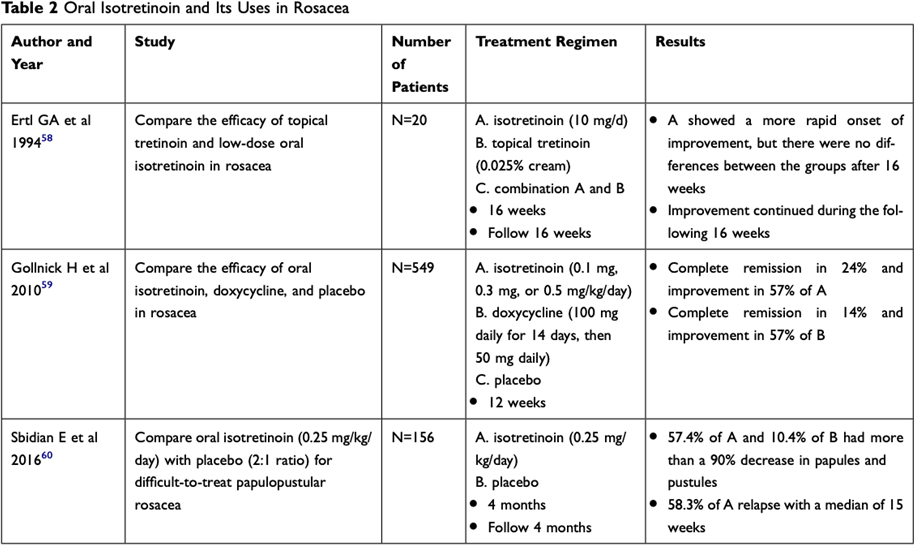
A recent paper has been published which looks at all the medical evidence for low dose oral isotretinoin therapy in rosacea. The purpose of this meta-analysis and systematic review was to evaluate the effectiveness of low-dose isotretinoin in the treatment of rosacea. This type of review is a very high level of evidence as it is not just a study but a systematic review of multiple studies showing oral isotretinoin therapy efficacy in rosacea treatment. The conclusion of this review of medical research is quoted below:
In summation, the study has shown that rosacea can be treated effectively with low-dose isotretinoin even in patients with advanced levels of the disease by applying the prescribed dose once a week. Further, the intervention has also been shown to have fewer side effects on the patients. Therefore, this study recommends RCTs be conducted to fully investigate the best combination options of the intervention for mild to severe rosacea based on the fact that some of the treatments combined have shown to be effective in the treatment of rosacea almost similar to that of low-dose isotretinoin.
This meta-analysis is available in its full format by clicking the link below.
Mechanism of Action of Oral Isotretinoin Therapy in Rosacea

Inhibition of sebaceous gland activity
Inhibition of the growth of Propionibacterium acnes within the follicle, although the retinoid is not antibacterial,
Inhibition of inflammation
Alteration of the pattern of keratinization within the follicle
Therefore, it is potentially the most effective long-term management therapy for chronic Type 2 and Type 3 rosacea sufferers. In fact, in Type 3 rosacea where patients develop rhinophyma and thickening of the skin its inhibition of sebaceous gland activity and shrinkage of the glands is the reason why it is the only drug that can help to treat and prevent this skin thickening. For example, it is very important that patients take oral isotretinoin after rhinophyma surgery to prevent recurrence of rhinophyma and skin thickening.
How is Oral Isotretinoin Taken in the Treatment of Rosacea
Although there is no official protocol oral isotretinoin dosing in rosacea is based around 0.3mg/kg dosing. This means that if you weigh 70 kilograms your daily dose in order to bring your symptoms under control for the first 6 months should be 20mg/day.
Once symptoms have settled and around 6 months of treatment are completed, in order to prevent relapse, a weekly isotretinoin maintenance (microdosing) can be continued to keep rosacea symptoms firmly at bay. Microdosing means taking a small amount of isotretinoin on a continual basis to prevent relapse of symptoms.

Example Rosacea Control dosing regimen Adult 70kg:
20mg orally once a day for 6 months
THEN
20mg twice weekly thereafter on going
OR
10mg alternate days ongoing
Dose Can Then be Further Reduced to a Minimum Controlling dose Weekly
70kg Patient as an example
20mg daily dose of oral isotretinoin for 6 months
After 6 months drop to a long-term maintenance dose of 20-30mg oral isotretinoin per week (eg. 10mg tablet taken twice or three times a week)
Please look at the final comments section at the end of the article for sample dosing guidelines for isotretinoin in rosacea.
Appropriate monitoring as per UK guidelines will be required.
If you feel that your rosacea is difficult to control and it is time to try more effective long term treatment then speak to one of our dermatologists at www.dermacne.co.uk.